A 59 year old male came with upper and lower weakness since 1 day
February 20, 2023
This is an online E logbook to discuss our patients' de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through a series of inputs from the available global online community of experts intending to solve those patients' clinical problems with the collective current best evidence-based inputs. This e-log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box are welcome.
Name:Manvitha (intern)
Chief complaints:
Right upper and lower weakness since 1 day
HOPI:
Patient was apparently asymptomatic till 1am of 19/2/2023 while watching TV he developed of weakness of right upper and lower limb and had H/O fall of remote from his hand with deviation of mouth to right side and slurring of speech
The weakness lasted for atleast 2-3 seconds and recovered after massage of right upper and lower limb
Then after 15min similar episode occurre again and he was shifted to nearby hospital where they suggested to nearby hospital by his attender
There is no H/O of LOC, Vomitings, fever
No involuntary passage of urine, no uprolling of eyes no tounge bite, no involuntary movements of limbs, no headache, no frothing through mouth , weakness not progressed
No fresh episode in the past
No similar episodes in the last
Past history
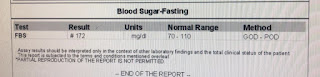
K/C/O DM 2 since 4 months on medication T. Metformin(500mg)+ T Glimiperide (1mg)
HTN diagnosed yester During the episode
Personal history
Diet mixed
Appetite decreased relieved on medication
Sleep adequate
Bowel and bladder regular
No known allergies
Habits:regularly takes alcohol 90ml/day stopped 1 month back
Family history: no significant family history
General examination:
Patien is conscious coherent cooperative
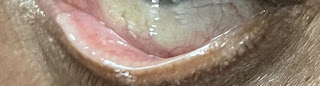
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema
Vitals:
PR:65bpm
BP: 200/80 mmHg
RR:46 cpm
Spo2:98%
GRBS:238mg/dl
CVS examination:
S1,S2 heard
No additional sounds heard
RS examination: position of trachea central
BAE +, NVBS +
Per abdomen:
Swelling seen over the umbilicus
Soft in consistency
Site at umbilicus area
Size 4X5 cm
Shape circular
Surface smooth
Skin over the swelling normal
Surrounding area normal
Shape of abdomen obese
No tenderness
No palpable mass
No organomegaly
Clinical images
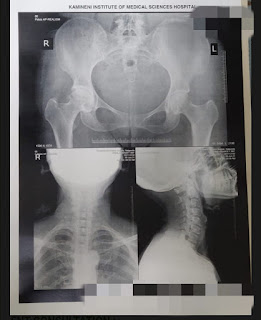
Investigations:












Comments
Post a Comment