56 yrs old female came to OPD with epigastric pain since 1 week.
8th June, 2021.
This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputsThis e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome
56 yrs old female came to OPD with epigastric pain since 1 week.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Following is the view of my case :
Case admitted under unit 2
History was taken by
Dr.A. Vaishnavi Mam PG y2
Dr. M. Vinay Sir PG y1
and helped by the interns
- G.Sai Vittal Sir
- Ch.Rishik Sir
- G.Preethi Mam
- Deekshitha Mam
CASE PRESENTATION
Chief complaints
Epigastric pain burning type since 5yr(on and off) Regurgitation symptoms since 1 week
HISTORY OF PRESENT ILLNESS
PAST HISTORY
5 years back she had chief complaints of pain in right hypochondrium diagnosed with cholelithiasis.
No history of Hypertension, Diabetes mellitus, Epilepsy, Tuberculosis, Coronary artery disease , CUA.
PERSONAL HISTORY:
Diet : Vegetarian
Appetite : Normal
Sleep : Adequate
Bowel and bladder : Regular
Micturition : Normal
No addictions
FAMILY HISTORY:
Not significant.
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative.
She is well oriented to time, place and person.
She is moderately nourished.
No Pallor
No Icterus
No Cyanosis
No Clubbing
No Lymphadenopathy
No Edema
VITALS:
Cardiovascular system : S1, S2 is heard. No murmurs are heard.
Respiratory system : Bilateral air entry is present, Normal vesicular breath sounds are heard. No adventitious sounds are heard.
Per Abdomen : Soft, Non-tender
CNS EXAMINATION: intact
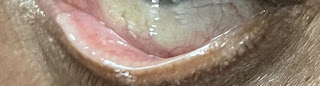
DENTAL CONSULTATION:
Chief complains: of ulceration on tongue and palate mucosa
On examination: no frank ulceration
Treatment tab Zincovit
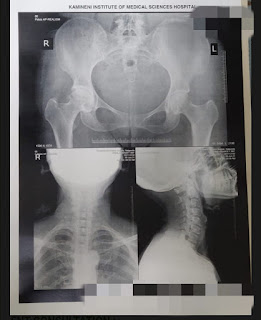
RADIOLOGICAL CONSULTATION
Brief Clinical details - Pain in the left hip region since 7 years known case spondyloarthropathy.
? SLE
Multiple join involvement present
Provisional diagnosis : ? SLE
Investigations: MRI for both hips bilateral
Region of interest/Special procedures : bilateral hips
ORTHOPAEDIC CONSULTATION
50 year old female having history of spondyloarthropathy since 7 years
Chief complaints of :
Pain at left hip since 7 years
History of cervical pain, left Knee joint pain
No history of fever
On Examination:
Patient is conscious, coherent, cooperative
GC - fair
CVS - S1and S2 sounds heard
CN - NAD
P/A - soft and non tender
RS - BAE+
On local Examination of left Hip:
No swelling
Tenderness at terminal flexion
ROM- Terminal flexion painful
Abduction upto 150 degrees
Flexion is limited
Treatment:
Review Reports
ENT CONSULTATION :
On examination of Oropharynx :-
PPW- Granular congested
Anterior pillar - Normal
Posterior pillar - Normal
Uvular/ soft palate - Normal
Posterior 1/3rd of tongue - Normal
No Palpable Lymphnodes
Provisional diagnosis :-
Acute pharyngitis with GERD
Treatment :-
1. Injection Pantop.
2. Life style modifications
3. Warm water gargles 3 to 4 times / day
SURGICAL CONSULTATION:
Patient was presented to OPD at 3:40pm patient came with
Chief complaints of
1) Pain in right hypochondrium since 2 months chief complaint of belching since 2 months complain of nausea on and off
No history of vomiting patient was apparently asymptomatic 2 months ago then she developed pain in right hypochondrium which was sudden in onset, gradually progressive, colicky type pain radiating to right scapula and intrascapular region with no Aggravating and relieving factors
Compliant of belching no history of vomitings, loose stools , constipation history of similar complaints in the past Gallbladder stones - 3mm, 5 years back
No history of any Any Surgeries. Not a known case of diabetes Mellitus, hypertension, CAD , CKD, thyroid disorder
On examination : conscious, coherent, cooperative
Temperature : afebrile.
Bp-130/80 mmhg
PR- 80bpm
Heart sounds -S1 S2 sounds heard
Respiratory- BAE positive clear
Per abdomen - soft, non tender, No guarding,rigidity
Impression - Asymptomatic cholelithiasis
Plan : Open/ LAP cholecystectomy
Treatment:
CST as per physician order
Tab DOLO 650 mg/PO/SOS
GYNAECOLOGY CONSULTATION
56 old P2L2A5 Post menopausal came with incidental findings from outside scan report showing left ovarian simple cyst measuring 1.5 x 1.3cm
No history of pain abdomen , white discharge
Complaint of Burning micturition (on and off) since 1 year
No history of Dysuria, nocturia
Known case of Gastritis and on antacids since 5-6 years
No history of post coital bleeding
Past history
No history of major surgeries in the past
No history of fever, cold , cough, vomiting , loose stools, constipation
Not a known case of hypertension, diabetes mellitus, TB, Epilepsy, bronchial asthma , CAD,CUD, Thyroid disorders
Family history of Gall bladder carcinoma to mother
Reached menopause 6 years back
Previous menstrual history
AOM - 13 years
8/30 , Regular
No pain
Marital history
Married life - 40 yrs
Non Consanguine marriage
OBS history
P1L1- male, 35 years , FTNVD( full term normal vaginal delivery)
A1- spontaneous at 1and a half month
P2L2- female, 30yrs FTNVD( full term normal vaginal delivery)
A2A3A4- Spontaneous at second month
Non Tubectomised
On Examination :-
Gc - fair
Temp- Afebrile
Bp - 130/80mmHg
Pulse rate - 73 bpm
Systemic examination
H/l - S1 and S2,
Respiratory system - BAE +
Per abdomen - soft , non tender
P/S - cervix : Healthy
Vagina : Healthy, no diseases
P/U - Uterus : Anteverted , normal size, mobile, non tender
B/L fornices free, non tender
56 yr old P2 L2 A5 post menopausal non- tubectomised with simple ovarian cyst left side
Advice :-
As the cyst size is 1.6 x 1.3 cm which is a functional type ( functional cyst)
< 6cm of cyst size. No active gynecological intervention required. Only observation is required with following scans for every 3 months to look for the size of cyst.
PAP taken - 2477
USG abdomen and pelvis :
Uterus - post menopausal status
Right and left ovaries - not visualised
Gastro Enterology Consultation.
Esophagus: Lax LES, Hills grade 1
Stomach : Atrophic Fundus mucosa seen , erythema in antrum
Duodenum : cap normal, D2 normal
Impression :
LaxLES
Atrophic fundal gastritis
Erythematous antral gastritis
INVESTIGATION:
Complete blood picture
Complete urine examination
LFT
RFT
Hemogram
Serum iron
Ferritin
Random Blood sugar
PROVISIONAL DIAGNOSIS
GERD( Gastroesophageal reflux disease)









Comments
Post a Comment