A 47yrs old patient came with chief complaints of decreased urine output and anasarca since 5 days
28th November , 2021.
This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputsThis e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome
A 47yrs old patient came with chief complaints of decreased urine output and anasarca since 5 days
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE PRESENTATION
Chief complaints
Pedal edema , facial puffiness since 6 days
Shortness of breath since 6 days increased since 3 days
Decreased urine output since 3 days
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 8 years back
8 years ago on regular checkup found to be hypertensive
6 years ago complaint of generalised weakness , weight loss diagnosed to be diabetic
5 years ago he had acute pancreatitis
6 days back patient developed pedal edema , progressed gradually associated with facial puffiness
Decreased urine output since 6 days , shortness of breath since 6 days grade 2 to 3 progressed to grade 4 since 3 days associated with orthopnea , PND , decreased appetite
No history of fever ,cold , cough , burning micturation , chest pain , giddiness , palpitations
PAST HISTORY
Diabetes , put on Tab. Glimi M2 PO BD since 6 years
Hypertension, put on Tab. Omesartan 20 OD since 8 years
History of acute pancreatitis 5 years ago
PERSONAL HISTORY:
Diet : Mixed
Appetite : Normal
Sleep : Adequate
Bowel and bladder : Regular
Micturition : Normal
Addictions:
alcohol stopped 5 years ago
smoking stopped 5 years ago
FAMILY HISTORY:
Not significant.
GENERAL EXAMINATION:
Patient is conscious cooperative coherent
well oriented to time place person and moderately built and moderately nourished
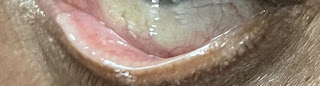
pallor present
no icterus
no cyanosis
no clubbing
Pedal edema present
no lymphadenopathy
VITALS:
Cardiovascular system : S1, S2 is heard. No murmurs are heard.
Respiratory system :
BAE present , crepitus present
CNS : intact
Per Abdomen : Soft, distended,
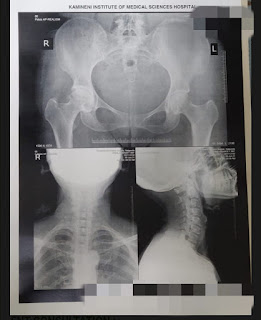
Clinical images
INVESTIGATION:
Complete urine examination
Hemogram
Colour Doppler 2D echo
Ultrasound report
Urine protein creatine ratio
Serum electrolytes
ABG
Renal function test
Serum creatinine
Liver function test
Blood urea
Blood sugar random
ECG
Anti HCV antibody
HBsAg rapid test
PROVISIONAL Diagnosis
Chronic kidney disease with type 2 diabetes Mellitus with diabetic nephropathy




















Comments
Post a Comment