A 50 years male came with Abdominal distension
This is an online e log book to discuss our patient’s de- identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patient’s clinical problems with collective current best evidence based inputs. This e-log book reflects my patient centered online portfolio and your valuable inputs on the comments is welcome.
June 10, 2022
Name : Lakshmi Manvitha Yechuri
Hall ticket no: 1701006096
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
CASE PRESENTATION :
HISTORY :
A 50 year old male patient who is a farmer and a daily wage worker by occupation, a resident of Pochampally, came to the opd with
CHIEF COMPLAINTS :
There is no local rise of temperature.
No hepatomegaly. No splenomegaly.
Guarding is present.
Rigidity is absent.
Kidney not palpable.
Shifting dullness : Positive
Liver span could not detected
Auscultation :
Bowel sounds are decreased.
Cardiovascular System : S1, S2 heard
Respiratory System : Normal vesicular breath sounds heard
Central Nervous System : Conscious; Speech normal ; Motor and sensory system examination is normal, Gait is normal.
INVESTIGATIONS :
1. Hemogram :
Hemoglobin : 9.8g/dl
TLC : 7,200
Neutrophils : 49%
Lymphocytes : 40%
Eosinophils : 1%
Basophils : 0%
PCV : 27.4%
MCV : 92.3 fl
MCH : 33 pg
MCHC : 35.8%
RDW-CV : 17.6%
RDW-SD : 57.8 fl
RBC count : 2.97 millions/mm3
Platelet count : 1.5 lakhs/mm3
Smear : Normocytic normochromic anemia
2. Serology :
HbsAg : Negative
HIV : Negative
3. ESR :
15mm/1st hour
4. Prothrombin time : 16 sec
5. APTT : 32 sec
6. Serum electrolytes :
Sodium : 133 mEq/L
Potassium : 3 mEq/L
Chloride : 94 mEq/L
7. Blood Urea : 12 mg/dl
8. Serum Creatinine : 0.8 mg/dl
9. LFTs :
Total Bilirubin : 2.22 mg/dl
Direct Bilirubin : 1.13 mg/dl
AST : 147 IU/L
ALT : 48 IU/L
ALP : 204 IU/L
Total proteins : 6.3 g/dl
Serum albumin : 3 g/dl
A/G ratio : 0.9
10. Ascitic fluid :
Protein : 0.6 g/dl
Albumin : 0.34 g/dl
Sugar : 95 mg/dl
LDH : 29.3 IU/L
SAAG : 2.66 g/dl
11. Ascitic Fluid Cytology :
12. Ascitic fluid culture and sensitivity report :
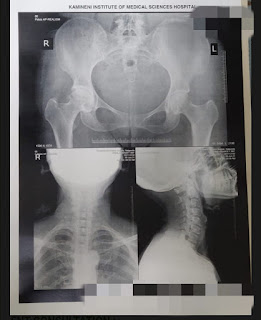
13. Ultrasound :
Coarse echotexture and irregular surface of liver - Chronic liver disease
Gross ascites
Gallbladder sludge
14. ECG
PROVISIONAL DIAGNOSIS :
Decompensated Chronic liver disease with ascites most likely etiology is alcohol.
TREATMENT :
Drugs :
1. Inj. Pantoprazole 40 mg IV OD
2. Inj. Lasix 40 my IV BD
3. Inj. Thiamine 1 Amp in 100 ml IV TID
4. Tab. Spironolactone 50 mg BB
5. Syrup Lactulose 15 ml HS
6. Syrup Potchlor 10ml PO TID
7. Fluid restriction less than 1L/day
8. Salt restriction less than 2g/day








Comments
Post a Comment