This is an online e log book to discuss our patient’s de- identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patient’s clinical problems with collective current best evidence based inputs. This e-log book reflects my patient centered online portfolio and your valuable inputs on the comments is welcome.
LONG CASE
June 10, 2022
Name : Lakshmi Manvitha Yechuri
Hall ticket no: 1701006096
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
Following is the view of my case :
CASE PRESENTATION:
A 59 years old female who is a house maker , resident of Nalgonda has presented to the opd with the chief complaints of
- Generalised weakness since 6 months
- Facial puffiness since 6 months
- Decreased urinary output since 3 months
Time line of events
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 1year back later she went to a local rmp for regular checkup and there she was diagnosed with hypertension and was on medication
Tab nifidepine 10mg
Tab furosemide 40mg
Patient complained of body pains 1year back she used analgesic
6 months back patient complaint of decreased food intake , weakness , puffiness of face and legs so went to near by hospital. But there was no improvement
5 months back they went to Miralguda hospital with reduced food intake, weakness, puffiness of face, Patient complained of bilateral pedal edema of grade 2 below the knees which was insidious in onset, gradually progressive, pitting type, increased as the day progressed and had no relieving factors
No history of nausea and vomiting.
and reduced urinary output doctor told that her kidneys were not functioning properly so she was put on medication as there was no improvement
They came to Kamineni Hospital in the month of April
Here the patient was put on dialysis which was
done weekly 2 times.
DAILY ROUTINE :
Patient usually wakes up at 5 am and will do household works and have breakfast along with coffee at 8am again continues her household work and then she will have her lunch which is rice, dal at 1:00pm and then takes a nap again continues her work then will have her dinner which is rice and dal at 8:30pm and goes for sleep at 10:00 pm.
PAST HISTORY
Known case of hypertension since 1yr
Not a known case of Diabetes mellitus , tuberculosis , asthma, epilepsy
No history of similar complaints in the past
No previous surgical history
PERSONAL HISTORY
Diet- Mixed
Appetite- Decreased since 1 month
Bowel and bladder movements- Urine frequency is reduced since 3 months
Bowel movements are regular
Sleep- Adequate
Addictions- no
No history of drug or food allergies
FAMILY HISTORY
No similar complaints in the family
GENERAL EXAMINATION
Done after obtaining consent, in the presence of attendant with adequate exposure
Patient is conscious, coherent, cooperative and well oriented to time, place and person
Patient is not well nourished and not moderately built
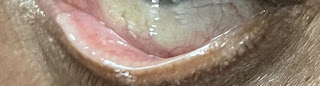
Pallor present
Pedal edema- present- bilateral pitting type
No history of cyanosis, clubbing and lymphadenopathy
Vitals
Temperature- Afebrile
Blood pressure- 150/90 mm of Hg
Pulse rate- 86 bpm
Respiratory rate- 21cpm
SpO2 : 98% At room air
SYSTEMIC EXAMINATION
1. Abdominal examination
On inspection
Shape of abdomen : distended
Umbilicus : inverted
Movements of abdomen wall with respiration
Skin is smooth and shiny
No visible peristalsis, pulsations, sinuses, engorged veins, hernial sites
On palpation
Inspectors findings are confirmed
Soft and non tender
No palpable mass
Liver and spleen not palpable
On percussion
Dull note
On auscultation
Bowel sounds heard
Cardiovascular system examination:
S1 and S2 sounds are heard
No murmurs
Respiratory system examination:
Bilateral air entry present
Normal vesicular breath sounds are heard
Central nervous system examination:
No focal neurological deficits
Investigations
Hemoglobin :- 4.5 gm/dl
Total count :- 7000 cells/cumm
Neutrophils :- 86%
Lymphocytes :- 12%
Eosinophils :- 0%
Monocytes :- 02 %
Basophils : 0 %
PCV :- 13.7 vol %
MCV :- 83.5 fl
MCH :- 27.4 pg
MCHC :- 32.8 %
RDW-CV :- 15.8 %
RDW -SD :- 47.5 fl
RBC count :- 1.64 millions/ cumm
Platelet count :- 28000
Impression :- Normocytic normochromic anemia with neutrophilia, thrombocytopenia
RFT
Urea :- 69 mg /dl (12-42mg/dl)
Creatinine :- 4.6 mg/dl (0.6-0.1)
Uric acid :- 3.9mg/dl (2.6-6)
Calcium :- 8.4mg/dl (8.6-10.2)
Phosphorus :- 3.5mg/dl (8.6-10.2)
Sodium :- 139mEq/L (136-145)
Potassium :- 3.4mEq/L (3.5-5.2)
Chloride :- 97mEq/L (98-107)
Provisional Diagnosis:
Chronic kidney disease on MHD secondary to hypertensive nephropathy ?
TREATMENT
2nd June
1. Tab Nodosis 550mg/PD/TID
2. Tab Pantoprazol 40mg /PR/OD
3. Tab Lasix 4mg/Pd/BD
4, Tab Nicardia 10mg/PO/BD
5. Tab Orofer XT/PO/OD
6. Tab Arkamin 0.1mg/PD/OD
7. Tab Zofer 4mg /PD/SOS
8. Tab MVT /PD/OD
9. 2 PRBC 1 SDP Reserve
10. 1 PRBC intradialysis transfusion
11. 1 SDP Transfusion
3rd June
1. Tab Nodosis 550mg/PD/TID
2.Tab Pan 40mg /PR/OD
3.Tab Lasix 4mg/Pd/BD
4.Tab Orofer XT/PD/OD
5.Tab Nicardia 10mg/PO/BD
6.Tab Arkamin 0.1mg/PD/OD
7.Tab Zofer 4mg /PD/SOS
8.Tab MVT/ PD/OD
9. 1 PRBC reverse and 1 SDP Transfusion
10. Inform SOS
11. 1 PRBC transfusion intradialysis
4th June
1.Tab Nodosis 550mg/PD/TID
2.Tab Pan 40mg /PR/OD
3.Tab Lasix 4mg/Pd/BD
4.Tab Orofer - XT/PD/OD
5.Tab Nicardia 10mg/PO/BD
6.Tab Arkamin 0.1mg/PD/OD
7.Tab Zofer 4mg /PD/SOS
8.Tab MVT /PD/OD
9. 1 PRBC intra dialysis planned for tomorrow morning
5th June
1.Tab Nodosis 550mg/PD/TID
2.Tab Pan 40mg /PR/OD
3.Tab Lasix 4mg/Pd/BD
4.Tab Orofer - XT/PD/OD
5.Tab Nocardia 10mg/PO/BD
6.Tab Arkamin 0.1mg/PD/OD
7.Tab Zofer 4mg /PD/SOS
8.Tab MVT /PD/OD
6th June
1.Tab Nodosis 550mg/PD/TID
2.Tab Pan 40mg /PR/OD
3.Tab Lasix 4mg/Pd/BD
4.Tab Orofer XT/PD/OD
5.Tab Nocardia 10mg/PO/BD
6.Tab Arkamin 0.1mg/PD/OD
7.Tab Zofer 4mg /PD/SOS
8.Tab MVT /PD/OD
7th June
1.Tab Nodosis 550mg/PD/TID
2.Tab Pan 40mg /PR/OD
3.Tab Lasix 4mg/Pd/BD
4.Tab Orofer - XT/PD/OD
5.Tab Nocardia 10mg/PO/BD
6.Tab Arkamin 0.1mg/PD/OD
7.Tab Zofer 4mg /PD/SOS
8.Tab MVT /PD/OD
8th June
1.Tab Nodosis 550mg/PD/TID
2.Tab Pan 40mg /PR/OD
3.Tab Lasix 4mg/Pd/BD
4.Tab Orofer XT/PD/OD
5.Tab Nocardia 10mg/PO/BD
6.Tab Arkamin 0.1mg/PD/OD
7.Tab Zofer 4mg /PD/SOS
8.Tab MVT /PD/OD
9th June
1.Tab Nodosis 550mg/PD/TID
2.Tab Pan 40mg /PR/OD
3.Tab Lasix 4mg/Pd/BD
4.Tab Orofer XT/PD/OD
5.Tab Nocardia 10mg/PO/BD
6.Tab Arkamin 0.1mg/PD/OD
7.Tab Zofer 4mg /PD/SOS
8.Tab MVT /PD/OD
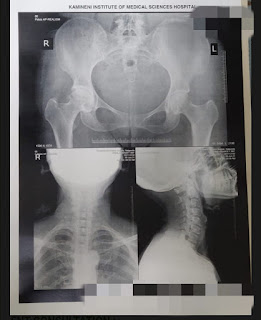
Instrument pictures

























Comments
Post a Comment