This is an online E logbook to discuss our patients' de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from the available global online community of experts intending to solve those patients clinical problems with the collective current best evidence-based inputs. This e-log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box are welcome.
Name: Lakshmi Manvitha Yechuri
Roll no: 169
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
CASE PRESENTATION:
A 20 yr old female, student by occupation has come to the OPD on 22nd march 2022 with the chief complaints of
- Abdominal pain since 7 am in the morning (22/3/2022)
- Vomiting since morning
History of presenting illness:
• Patient was apparently asymptomatic 7 days back then she developed pain in the epigastric region.
• It was sudden in onset, gradually progressive and is of squeezing type. There were no aggrevating and relieving factors.
• She also complain of 3 episodes of vomitings
1st episode :- she took medication for abdominal pain from pharmacist which was digiene and omidine after taking medicine at 7:15 Am she had 1st episode of vomiting which was non projectile , bilious, non foul smelling and no contents of food.
2nd episode :- After half an hour she took medicine for constipation which was given by pharmacist with in 2mins she had 2nd episode of vomiting which was non projectile, bilious, non foul smelling , no contents of food.
3rd episode :- she went to general surgeon in her hospital for vomiting she was put on normal saline with B complex she was not able to tolerate that smell and she had vomiting which was non projectile , bilious non foul smelling and contents of food (rice)
• Then general surgeon prescribed her zofer tablet
• That is how she came to the hospital around 12pm.
• She had history of epigastric pain 6 months back which was sudden in onset gradually progressive radiating to left flank then she went to near by hospital and was diagnosed as acute pancreatitis and took medication. after 1month she went to follow up they told that it got relieved so she stopped using medicine.
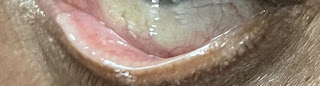
• After 10 days of epigastric pain she developed skin lesions on her lower limbs and buttocks. She went to RMP he gave ointment but it is not resolved, she also developed skin lesions over her forehead 4 months back.
•Patient had a history of RTA(fracture) to right leg 3 years back at the time of which she was diagnosed with diabetes mellitus type 1 and was advised to take subcutaneous insulin which she continued for 1 year and then discontinued the insulin as she was getting pain at the site of injection then she went to RMP he gave oral diabetic drugs she used them for 1 month as the blood glucose levels were not normal she again started using insulin 12u ---×---12u
She had irregular life styles since the past two months and on the night before epigastric pain, she took the insulin but did not have her dinner
Patient was not a known case of hypertension, asthma, thyroid, TB and epilepsy
No history of previous surgeries and blood transfusions
Personal history:
Diet- Mixed
Appetite- decreased
Sleep- Adequate
Bowel and bladder- Regular
Addictions- None
Menstrual history:
Menarche-12 yrs
Regular cycles - 5/30
Not associated with pains, clots and foul smelling
Since 1 month she complaints of spotting PV
Family history:
Her paternal grand mother was diagnosed with diabetes
No other significanf family history
Allergic history:
No history of any allergies to drugs or any food
General physical examination:
Patient was conscious, coherent and cooperative and well oriented to time, place and person
Moderately nourished and built
No pallor, icterus, cyanosis, clubbing, generalized lymphadenopathy, edema
Vitals:
Temperature- Afebrile
Blood pressure- 110/80mm of Hg
Pulse rate- 94 bpm
Respiratory rate- 18/min
SPO2- 99%
GRBS- 215 mg%
Systemic examination:
Per abdomen examination:
Inspection:
On inspection, abdomen appears to be scaphoid in shape umbilicus is inverted
Multiple scars are seen around the umbilicus
No sinuses, engorged veins, visible peristalsis and pulsations
Palpation:
Inspectory findings were confirmed
No local raise of temperature
No tenderness
No guarding and rigidity
No hepatospelnomegaly
Percussion:
Tympanic note heard
Auscultation:
Bowel sounds are present
CVS:
S1 and S2 were heard and no murmers
Respiratory system:
Bilateral air entry is present.
Normal vesicular breath sounds were heard
CNS:
No neurol focalogical deficits
Investigations:
Complete blood picture:-
Complete urine examination:-
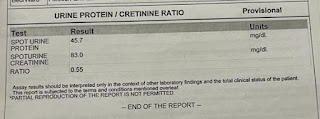
Urine protein - creatinine ratio
Urine for ketone bodies :-
Liver function test :-
Random blood sugar :-
ABG:-
ECG:
2D echo:
USG:
CT:
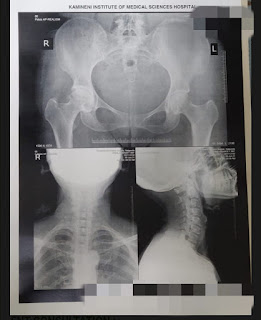
Chest x-ray:
Provisional diagnosis:
Acute Pancreatitis with DKA with Type 1 Diabetes Mellitus (since 3 years) secondary to hypertriglyceridemia
TREATMENT
Day 1:-
1. Nbm till further orders.
2. IVF- NS & RL @ 150ml/hr.
3. Inj HAI ( 39ml Normal Saline + 40 IU HAI ) @ 4 ml / hr according to Algorithm
4. Inj. Pantop 40mg/IV/OD.
5. Inj. Zofer 4mg/IV/OD.
6. Inj. Tramadol 1amp in 100 ml/NS/IV/BD.
7. Inj. THIAMINE 2amp in 1 NS/IV/TID.
8. Monitor vitals.
9. Measure abdominal girth
Day 2
No Fresh Complaints
Patient is conscious,coherent,cooperative
vitals :
Temp - afebrile
BP - 110/80 mm hg
PR - 99 bpm.
RR - 18 cpm
spo2 - 100 @RA
GRBS - 222 mg/dl @ 8 am
CVS - S1, S2 heard
RS - bae present
P/A - Soft , Non tender
bowel Sounds - Present
Stools - Not Passed
CNS - NAD
I/O - 2000/1800 ml
Rx
NBM
IVF- NS & RL @ 100 ml/hr.
Inj Pantop 40mg/IV/OD.
Inj. Zofer 4mg/IV/SOS.
Inj. Tramadol 1amp in 100 ml/NS/IV/ SOS
Inj. THIAMINE 2amp in 1 NS/IV/TID.
Monitor vitals.
Day 3
No Fresh Complaints
Patient is conscious,coherent,cooperative
vitals :
Temp - afebrile
BP - 110/80 mm hg
PR - 75 bpm.
RR - 18 cpm
spo2 - 100 @RA
GRBS - 215 mg/dl @ 8 am
CVS - S1, S2 heard
RS - bae present
P/A - Soft , Non tender
bowel Sounds - Present
Stools - Not Passed
CNS - NAD
Rx:-
I/O - 1500/1300 ml
Oral Sips Of water Given
IVF- NS & RL @ 100 ml/hr.
Inj Pantop 40mg/IV/OD.
Inj. Zofer 4mg/IV/SOS.
Inj. Tramadol 1amp in 100 ml/NS/IV / SOS
Inj. Optineuron 1amp in 100ml NS/IV/OD
Monitor vitals.
Day 4:-
No Fresh Complaints
- Patient is conscious,coherent,cooperative
vitals :
Temp - afebrile
BP - 110/80 mm hg
PR - 72 bpm.
RR - 18 cpm
spo2 - 100 @RA
GRBS - 243 mg/dl @ 7 am
CVS - S1, S2 heard
RS - bae present
P/A - Soft , Non tender
bowel Sounds - Present
Stools - Passed
CNS - NAD
Rx
Oral feeds allowed
IVF- NS & RL @ 100 ml/hr.
Inj Pantop 40mg/IV/OD.
Inj. Zofer 4mg/IV/SOS.
Inj HAI acc to GRBS TID / SC
Inj. Tramadol 1amp in 100 ml/NS/IV / SOS
Inj. Optineuron 1amp in 100ml NS/IV/OD
Monitor vitals.
Dermatology refferal:-
Gynecology refferal :-

































Comments
Post a Comment